Hi , I am Samhitha ,5th semester student. This is an online elog book to discuss our patients health data after taking his consent. This also reflects my patient centered online learning portfolios
Hi, I am p.samhitha, 5th Sem Medical Student.This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
PLAN OF TREATMENT-
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.”
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS
Pt came with
-c/o giddiness since 1 yr
-c/o headache since 1 yr
HISTORY OF PRESENTING ILLNESS:
Pt was apparently asymptomatic 1 yr ago then she developed giddiness which is associated with sweating palpitations
C/o headache which is throbbing in temporal region and not associated with photophobia phonophobia and nausea
No h/o giddiness aggravating with neck movements earache and tinnitus
No h/o vomiting fever loose stools pain abdomen cough cold
No h/o slurring of speech limb weakness deviation of mouth
No h/o sob chest pain palpitations orthopnea pnd
PAST HISTORY:
K/C/O DM 2 since 1 yr (on tab metformin 500 mg) ,HTN since 1 yr (on omlesartan 20 mg )and CVA since 1 yr (on atrozio gold (atrovastatin clopidogrel and aspirin))
(CT scan - B/l periventricular white matter hypodensities ? Chronic Ischemic changes
Multiple small calcific foci in the frontal and b/l parietal region)
N/k/c/o TB , Epilepsy, CAD
PERSONAL HISTORY:
Diet - Mixed
Appetite - Normal
Bowel and Bladder movements- Regular
Sleep - Adequate
Addictions - None
FAMILY HISTORY-
Not significant
GENRAL EXAMINATION-
Pt is c/c/c well oriented to time place and person
No signs of pallor icterus cyanosis clubbing lymphadenopathy edema
Temp - Afebrile
PR - 78bpm
RR - 18cpm
BP - 110/80mmhg
Spo2 - 98RA
GRBS - mg%
SYSTEMIC EXAMINATION-
CVS -
S1 S2 +
No thrills felt
No murmurs heard
RS -
B/l air entry +
Position of trachea central
No wheeze or rhonchi
P/A-
Shape - scphaoid
No tenderness or organomegaly present
CNS-
She is conscious coherent and cooperative
No signs of meningeal irritation
Motor System-
GCS 15/15 - E4V5M6
Power-
R. L.
U/l 5/5. 5/5
L/l. 5/5. 5/5
Tone-
U/l. N. N
L/l. N. N
Reflexes-
B. +. +
T. + +
K. - -
A. - -
Plantar Flexor. Flexor
PROVISIONAL DIAGNOSIS-
Giddiness under evaluation ?Hypoglycemia
H/o CVA 1 yr ago
INVESTIGATIONS-
CUE -
Alb - Nil
Sugar - Nil
Pus cells - 1-2
Epithelial cells - 2-3
Rbc - nil
HEMOGRAM-
Hb - 8.4
Tlc - 5900
Platlets - 2.88
Rbs - 117
Blood urea - 42
Sr . Creat - 1.5
USG -
B/l Grade 1 RPD changes
Grade 1 Fatty liver
2D echo -
Trivial TR
No MR AR
No RWMA
No AS/MS sclerotic
Good LV systolic function
Diastolic dysfunction
No
Ecg-
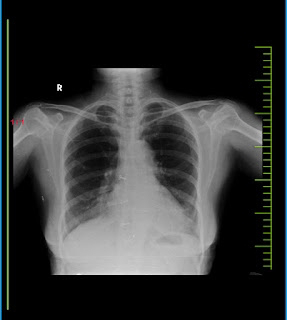
Chest X-Ray
PLAN OF TREATMENT-
Tab Ecosprin PO/OD
Tab Metformin 500 mg
Tab Omelsartan 20 mg